Abstract
APVO436 is a recombinant T-cell engaging humanized bispecific antibody designed to redirect host T-cell cytotoxicity in an MHC-independent manner to CD123-expressing blast cells from patients with hematologic malignancies. We evaluated the risk, severity, and biomarkers of treatment-emergent cytokine release syndrome (CRS) in patients with relapsed/refractory (R/R) acute myeloid leukemia (AML) or myelodysplastic syndrome (MDS) who received APVO436 during the dose escalation phase of a Phase 1B study (ClinicalTrials.gov identifier: NCT03647800). A total of 46 R/R AML/MDS patients received single agent APVO436 as weekly intravenous infusions at 10 different dose levels, ranging from 0.3 mcg to 60 mcg.
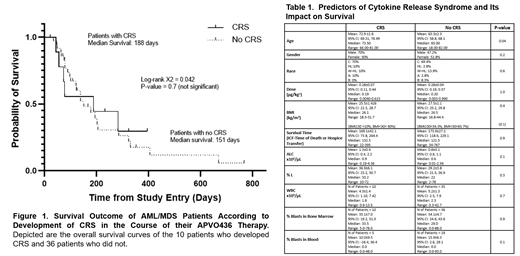
CRS was the 7th th most common AE after pyrexia, diarrhea, infusion related reaction, peripheral edema, fatigue, and anemia affecting 10 (21.7%) of the 46 patients. Grade 3-4 CRS was the 6 th most common Grade ≥3 AE following febrile neutropenia, anemia, hyperglycemia, decreased platelet count, and sepsis occurring in 4 of the 46 patients (8.7%) treated with APVO436 in Study 5001 regardless of any relationship with the study drug APVO436. CRS was reported as an SAE in 7 (70%) of the 10 patients who developed CRS. CRS lead to dose interruptions in 4 patients, dose reduction in 1 patient, and permanent discontinuation of the study drug in 1 patient. Only 2 of the 46 patients experienced DLT and it was related to CRS in both patients. One patient treated in Cohort 4 who developed grade 2 CRS died due to complications from acute renal failure. Notwithstanding the fact that it is a potentially life-threatening complication, CRS did not significantly affect the overall survival outcome of the safety population (Figure 1). The average survival times were 169.1±42.1 days for patients who developed CRS and 173.9±27.2 days for the remainder of patients (P=0.9) (Table 1). The median survival was 188 days for patients with CRS and 151 days for those without CRS (Log-rank C 2 = 0.042, P=0.7) (Figure 1).
Premedication with steroids (Dexamethasone) did not eliminate the risk of CRS. Of 4 patients who developed Grade ≥3 CRS, 2 had received steroid prophylaxis. Notably, CRS did not show an apparent dose-relationship. The average dose levels were 0.28±0.21 (Median: 0.19) µg/kg for those patients who developed CRS and 0.28±0.27 (Median: 0.20) µg/kg for those who did not develop CRS (P=0.97). There was a borderline significant age difference between patients who did versus patients who did not develop CRS (72.9±1.6 years [Median 73.5 years] vs. 63.3±2.3 years [Median: 65.0 years] (P=0.04). Diagnosis, dose level, gender, race, obesity, or baseline hematologic parameters in peripheral blood did not predict the risk of CRS (Table 1). There was a statistically insignificant (P=0.1) trend toward higher absolute lymphocyte count (ALC) for patients who experienced CRS. Patients with a higher leukemia burden, as determined by higher total WBC, higher percentage of blasts in bone marrow, or higher percentage of blasts in peripheral blood did not have a higher incidence of CRS.
Cytokine profiling in select patients who developed Grade 2-4 CRS after APVO436 infusion indicates that the predominant cytokine in this inflammatory cytokine response is IL-6: Within 1-2 days following the first dose of APVO436, the mean serum IL-6 concentration was elevated 145-fold over baseline (755 vs 5.2) and at the end of one week it was still elevated 83-fold over baseline. APVO436-associated CRS was generally manageable with standard of care and in most cases it resolved rapidly with the administration of tocilizumab at standard doses combined with dexamethasone. APVO436-related CRS was not required for clinically meaningful responses in R/R AML patients, and it did not affect their survival outcome. Notably patients who developed CRS after APVO436 therapy were not more or less likely to have a favorable response. Among 8 patients with favorable responses, 4 experienced a CRS and 4 did not. APVO436-related CRS was not required for clinically meaningful responses in R/R AML patients, and it did not affect the survival outcome. Prolonged stabilization of disease, partial remissions and complete remissions were achieved in both patients who experienced CRS as well as patients who did not experience CRS after APVO436 infusions.
Lin: AbbVie, Aptevo Therapeutics, Astellas Pharma, Bio-Path Holdings, Celgene, Celyad, Genentech-Roche, Gilead Sciences, Incyte, Jazz Pharmaceuticals, Novartis, Ono Pharmaceutical, Pfizer, Prescient Therapeutics, Seattle Genetics, Tolero, Trovagene: Research Funding. Watts: Takeda: Consultancy, Research Funding; Genentech: Consultancy; Rafael Pharma: Consultancy; Celgene/BMS: Consultancy. Mims: Kura Oncology: Consultancy; Genentech: Consultancy; Abbvie: Consultancy; Syndax Pharmaceuticals: Consultancy; BMS: Consultancy; Jazz Pharmaceuticals: Consultancy; Daiichi-Saynko: Consultancy; Glycomemetics: Research Funding; Leukemia and Lymphoma Society: Consultancy; Aptevo: Research Funding; Xencor: Research Funding. Patel: Peerview: Honoraria; BMS-Celgene, Agios: Membership on an entity's Board of Directors or advisory committees; Aptevo Therapeutics: Research Funding. Shami: Chimerix: Research Funding; BMS: Consultancy; Gilead: Consultancy; Takeda: Consultancy; Chimerix: Research Funding; Bastion Biologics: Consultancy, Membership on an entity's Board of Directors or advisory committees; JSK Therapeutics: Consultancy, Current holder of individual stocks in a privately-held company, Membership on an entity's Board of Directors or advisory committees; Amgen: Research Funding; Aptevo: Research Funding. Cull: Aptevo: Research Funding. Cogle: Celgene: Membership on an entity's Board of Directors or advisory committees; Aptevo therapeutics: Research Funding. Lee: oncotelic therapeutics: Current equity holder in publicly-traded company; Aptevo therapeutics: Consultancy. Uckun: oncotelic therapeutics: Current equity holder in publicly-traded company; Aptevo therapeutics: Consultancy; Reven Pharmaceuticals (Reven LLC): Consultancy, Membership on an entity's Board of Directors or advisory committees.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal